Back and neck pain are among the most common reasons people seek medical care. Imaging results often reveal disc problems, but many patients feel confused when they hear terms like bulging disc or herniated disc. While these conditions are related, they are not the same—and understanding the difference can help guide treatment decisions and ease unnecessary worry.
This article explains how bulging and herniated discs differ, what symptoms they may cause, and what treatment options are available.
Understanding the Anatomy of a Spinal Disc
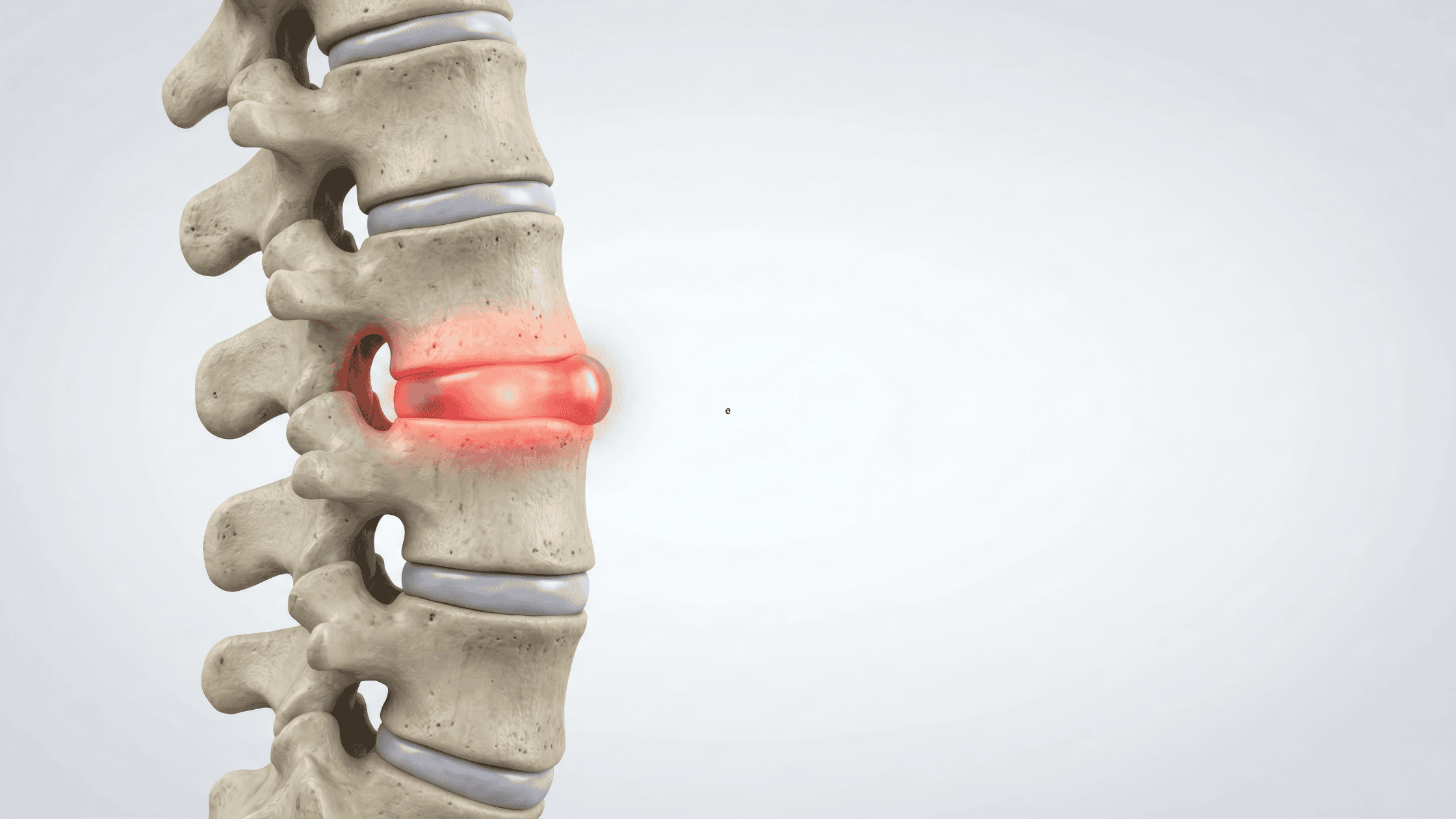
The spine is made up of vertebrae cushioned by intervertebral discs. Each disc has:
- A soft, gel-like center (nucleus pulposus)
- A tough outer layer (annulus fibrosus)
Discs act as shock absorbers and allow flexibility in the spine. When discs are stressed, injured, or degenerate with age, problems like bulging or herniation can occur.
What Is a Bulging Disc?
A bulging disc occurs when the disc extends beyond its normal boundary but the outer layer remains intact. Think of it as a tire that looks slightly overinflated—stretched, but not ruptured.
Key Characteristics:
- Often affects a broad area of the disc
- Common with age-related degeneration
- May not cause symptoms
- Frequently found incidentally on MRI
Many people have bulging discs without any pain at all.
What Is a Herniated Disc?
A herniated disc happens when a tear in the outer layer allows the inner gel to leak out. This material can irritate or compress nearby nerves, leading to more noticeable symptoms.
Key Characteristics:
- A focal tear or rupture
- More likely to cause nerve compression
- Can develop suddenly from injury or strain
- Often associated with pain, weakness, or numbness
Herniated discs are sometimes referred to as “slipped” or “ruptured” discs.
Key Differences Between Bulging and Herniated Discs
| Feature | Bulging Disc | Herniated Disc |
| Disc structure | Outer layer intact | Outer layer torn |
| Size of involvement | Broad, symmetrical | Localized, focal |
| Symptom severity | Often mild or none | More likely severe |
| Nerve compression | Less common | More common |
| Cause | Aging, posture, wear | Injury, degeneration, strain |
Common Symptoms (When Present)
Both conditions can be asymptomatic, but symptoms may include:
- Localized neck or back pain
- Radiating pain into arms or legs
- Numbness or tingling
- Muscle weakness
- Pain that worsens with movement, coughing, or sitting
Symptoms depend on disc location and whether nerves are involved.
How Are Disc Problems Diagnosed?
Diagnosis typically involves:
- Detailed medical history
- Physical and neurological examination
- Imaging such as MRI or CT scans
Importantly, imaging findings must match symptoms. Many disc abnormalities do not require treatment.
Treatment Options for Bulging and Herniated Discs
Conservative (Non-Surgical) Treatments
- Activity modification
- Physical therapy
- Anti-inflammatory medications
- Postural correction
- Pain-relieving injections
Advanced Interventional Options
- Epidural steroid injections
- Targeted nerve blocks
- Regenerative therapies (in appropriate cases)
Surgery (When Necessary)
Surgery is typically reserved for:
- Progressive neurological weakness
- Loss of bowel or bladder control
- Severe pain not responding to conservative care
Most patients do not require surgery.
Why the Distinction Matters
Understanding whether a disc is bulging or herniated helps:
- Set realistic expectations
- Avoid unnecessary fear
- Guide appropriate treatment plans
- Emphasize conservative care when appropriate
Disc findings alone do not define pain—function, symptoms, and quality of life matter most.
When to Seek Medical Care
You should consult a spine or pain specialist if you experience:
- Persistent or worsening pain
- Radiating pain with numbness or weakness
- Difficulty walking or using your arms
- Sudden loss of bladder or bowel control (emergency)
Final Thoughts
Bulging and herniated discs are common spinal findings, especially as we age. While they sound alarming, many people improve with conservative care and guided movement. A personalized evaluation is essential to determine whether disc findings are truly the source of pain—and what treatment path makes the most sense.
If you’re experiencing back or neck pain and have questions about your imaging results, a comprehensive, non-surgical evaluation can help you move forward with confidence.